
By the time a child crawls, he is blanketed by an enormous cloud of microorganisms.
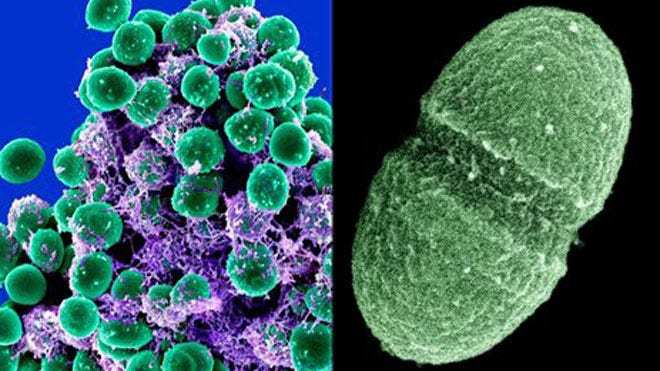
Helicobacter pylori may be the most successful pathogen in human history. While not as deadly as the bacteria that cause tuberculosis, cholera, and the plague, it infects more people than all the others combined. H. pylori, which migrated out of Africa along with our ancestors, has been intertwined with our species for at least two hundred thousand years. Although the bacterium occupies half the stomachs on earth, its role in our lives was never clear. Then, in 1982, to the astonishment of the medical world, two scientists, Barry Marshall and J. Robin Warren, discovered that H. pylori is the principal cause of gastritis and peptic ulcers; it has since been associated with an increased risk of stomach cancer as well. Until that discovery, for which the men shared a Nobel Prize, in 2005, stress, not an infection, was assumed to be the major cause of peptic ulcers.
H. pylori is shaped like a corkscrew and is three microns long. (A grain of sand is about three hundred microns.) It is also one of the rare microbes that live comfortably in the brutally acidic surroundings of the stomach. Doctors realized that antibiotics could rid the body of the bacterium and cure the disease; treating ulcers this way has been so successful that there have been periodic discussions of trying to eradicate H. pylori altogether. The consensus was clear; as one prominent gastroenterologist wrote in 1997, “The only good Helicobacter pylori is a deadHelicobacter pylori.” Eradication proved complicated and expensive, however, and the effort never gained momentum. Yet few scientists questioned the goal. “Helicobacter was a cause of cancer and of ulcers,’’ Martin J. Blaser, the chairman of the Department of Medicine and a professor of microbiology at the New York University School of Medicine, told me recently. “It was bad for us. So the idea was to get it out of our bodies, as fast as we can. I don’t know of anyone who said, Gee, we better think about the consequences.”
No one was more eager to rout the organism from the human gut than Blaser, who has devoted most of his working life to the study of H. pylori. His laboratory at N.Y.U. developed the first standard blood tests to identify the microbe, and most of them are commonly in use today. But Blaser, a restless intellect who, in addition to his medical duties, helped start the Bellevue Literary Review, wondered how an organism as old as humans could survive if it caused nothing but harm. “That isn’t how evolution works,” he said. “H. pylori is an ancestral component of humanity.” By the nineteen-nineties, Blaser had begun to look more closely at the bacterium’s molecular behavior, and in 1998 he published a paper in the British Medical Journalsuggesting, contrary to prevailing views, that it might not be so dangerous after all. The following year, he started the Foundation for Bacteriology, to help focus attention on the critical, and usually positive, role that these organisms play in human evolution.
“We have a certain narrative,’’ he said, sitting in his laboratory. A Tennessee license plate—“hpylori”—rested on his desk and a detailed map of the bacterium’s genome was hanging on a wall. Blaser, wearing a crisp blue sports coat, and with well-tended gray hair, projects an air of genial confidence; he seems more like the chief executive of a conglomerate than like the bench scientist he has been for decades. “Germs make us sick,” he said. “But everyone focusses on the harm. And it’s not that simple, because without most of these organisms we could never survive.’’
Since 1953, when James Watson and Francis Crick described the structure of DNA, we have looked upon genes as our biological destiny. The double helix provided a blueprint for life, and the process of making a human, while staggeringly complex, was also straightforward: genes manufacture proteins, which, in turn, build the various parts we need. When DNA is damaged or genes interact poorly with one another, the eventual result is disease. To understand how and when our genes malfunction, then, would be to understand how to prevent, treat, and cure everything from cancer to the common cold. That search became the central task of molecular biology. In the past decade, however, aided by the rapidly escalating power of computer processing and by the same revolution in DNA-sequencing technology that made it possible to map our genome, another truth has emerged: while our health is certainly influenced by genes, it may be affected even more powerfully by bacteria.
We inherit every one of our genes, but we leave the womb without a single microbe. As we pass through our mother’s birth canal, we begin to attract entire colonies of bacteria. By the time a child can crawl, he has been blanketed by an enormous, unseen cloud of microorganisms—a hundred trillion or more. They are bacteria, mostly, but also viruses and fungi (including a variety of yeasts), and they come at us from all directions: other people, food, furniture, clothing, cars, buildings, trees, pets, even the air we breathe. They congregate in our digestive systems and our mouths, fill the space between our teeth, cover our skin, and line our throats. We are inhabited by as many as ten thousand bacterial species; these cells outnumber those which we consider our own by ten to one, and weigh, all told, about three pounds—the same as our brain. Together, they are referred to as our microbiome—and they play such a crucial role in our lives that scientists like Blaser have begun to reconsider what it means to be human.
“I love genetics,” Blaser said. “But the model that places our genes at the root of all human development is wrong. By itself, it simply cannot explain how rapidly the incidence of many diseases has risen.” He stressed that genes matter immensely, but that one must take into account more than just the twenty-three thousand genes we inherit from our parents. The passengers in our microbiome contain at least four million genes, and they work constantly on our behalf: they manufacture vitamins and patrol our guts to prevent infections; they help to form and bolster our immune systems, and digest food. Recent research suggests that bacteria may even alter our brain chemistry, thus affecting our moods and behavior.
The process of learning about our microbiome is in its early days, but even the most tentative results have begun to transform our understanding of human health.Recently, a group at the University of Maryland School of Medicine identified twenty-six bacterial species that reside in the guts of members of the Old Order Amish sect—a closed population, with a nearly identical gene pool—that seem to account for common metabolic abnormalities such as high blood pressure and insulin resistance. Similar research has suggested that the destruction of bacteria may contribute to Crohn’s disease, obesity, asthma, and many other chronic illnesses. “The prospects here are endless,’’ Blaser said. “We need to be careful with the science and not oversell it. But I have been a practicing physician and medical researcher for more than thirty years, and this is the most exciting and important work of my lifetime.”
Bacteria have inhabited the earth for at least two and a half billion years. Our evolutionary ancestors arrived in a world dominated by microbes, and, as we evolved, so did they. Until recently, it was nearly impossible to sift through molecules and determine the impact that those organisms have had on us. Scientists first needed to locate a microbe in the body, then remove a sample and grow it in culture. With billions of cells to examine, the data could never be complete or even representative. DNA-sequencing technology changed that, opening the microbial world for the first time to sophisticated scrutiny. After the successful conclusion of the Human Genome Project, the National Institutes of Health launched a similar enterprise, in 2007, to map the human microbiome. For the past five years, scientists associated with the Human Microbiome Project have followed two hundred and forty-two healthy people, periodically sampling bacteria from their mouths, nasal passages, skin, and other sites on and in their bodies. In 2008, the European Commission and China joined the hunt, with the Metagenomics of the Human Intestinal Tract Project, known as Metahit.
Computers have made it possible for researchers to purify the DNA contained in thousands of samples and to separate bacterial from human genes. (Scientists know how to identify human DNA; when they discard it, genes from the microbiome remain.) The initial results, published this summer, opened a surprising window on the human body, detailing the vast range of microbes that colonize nearly every surface we have. Most reside within the gut, but many also occupy our mouths, and one particular bacterium, Streptococcus mutans, has been recognized as the principal cause of tooth decay. When you eat sugar, S. mutans releases acid that corrodes the teeth. Many researchers who study the microbiome now look upon cavities as an infectious disease, and they are testing a mouthwash that kills S. mutans; if it works, dental cavities could vanish. Microbial communities vary widely within and among people, yet they are also specific; the microbes found in your mouth, for instance, are far more likely to resemble the bacteria in another person’s mouth than the bacteria found in any other part of your body. But our microbial world is enormous, and it changes constantly: a recent study of a hundred and twenty-four people in Denmark and Spain found at least a thousand different species of gut microbes, although each person carried, on average, only a hundred and sixty species.
All animals have biomes. There is a cat microbiome, a dog microbiome, an alligator microbiome, and a dolphin microbiome. Earlier this summer, scientists in North Carolina State University’s Department of Poultry Science received a grant from the U.S. Department of Agriculture to study the chicken microbiome. Plants, too, need microbial communities to survive. Rhizobium, a bacterium that lives in nodules on the roots of legumes, helps its hosts carry out a series of chemical steps required to supply much of the earth’s nitrogen. “Like fifteenth-century explorers describing the outline of a new continent, Human Microbiome Project researchers employed a new technological strategy to define, for the first time, the normal microbial makeup of the human body,” Francis Collins, the director of the N.I.H., said when the project’s initial results were released, this summer. He called it a remarkable reference database that would lay “the foundation for accelerating infectious-disease research previously impossible without this community resource.”
The Human Microbiome Project has helped scientists identify many species and learn which parts of our bodies they colonize. But to understand what goes wrong when we are sick the researchers will need to determine how these organisms interact with one another and with us. Hardly a week goes by without a new symposium, a call for a special issue of a scientific publication, or the announcement of a grant intended to decipher the role of bacteria in any number of diseases. “We are in that beautiful, euphoric, heady early period,’’ David A. Relman, a professor of medicine, microbiology, and immunology at the Stanford University School of Medicine, said. Relman was the first to sequence the genomes of a human bacterial community—which happened to come from his own mouth. “We see this in any kind of newly emerging science. I keep trying to inject a bit of moderation, while not wanting to dampen the enthusiasm of a truly exciting time. So far, though, there are relatively few circumstances where you can meet a patient who is benefitting from this.” Relman argues that our biome is a complex and dynamic network, but one that, despite its importance, remains poorly understood. “We have to stop looking at medicine as a war between invading pathogens and our bodies,’’ he told me when we met at his office, at the V. A. hospital in Palo Alto, where he is chief of infectious diseases. “This sort of stewardship has more in common with park management than it does with our current practice of trying, in the broadest way possible, to kill microbes.”
Looked upon this way, the human body turns out to be a vast, highly mutable ecosystem—each of us seems more like a farm than like an individual assembled from a rulebook of genetic instructions. Medicine becomes a matter of cultivation, as if our bacterial cells were crops in a field. When that community is disturbed, either by the presence of an excess of bacteria like S. mutans, which causes cavities, or, more often, through the use of a powerful, broad-spectrum antibiotic, trouble can arise. Earlier this year, a team led by Susan Lynch, an associate professor of medicine at the University of California at San Francisco, reported that the bacteriumLactobacillus sakei may be singularly capable of warding off the painful sinusitis suffered each year by thirty million Americans; the incidence of sinusitis is far lower among people who retain that particular microbe, which is destroyed by antibiotics. In August, Ilseung Cho, of the New York University School of Medicine, published a study showing that antibiotics eradicated bacteria, commonly found in the digestive system of mice, that help the animals metabolize calories efficiently; without the microbes, the mice absorbed more calories from the same amount of food and rapidly became obese.
Anyone with a vegetable garden knows that herbicides will make quick work of your weeds; but, used the wrong way, they will do the same thing to your food. Antibiotics, it has become clear, are herbicides for humans. Medically, they are absolutely vital—but they also can alter our internal ecosystem in ways, both big and small, that even a decade ago seemed unimaginable.
Ridding our bodies of nasty microorganisms has been a goal of medicine at least since the invention of the microscope. The introduction of antibiotics, the signature medical achievement of the twentieth century, helped solidify that idea. Drugs such as penicillin and streptomycin have saved millions of lives, and we have come to see the world as a place filled with germs that ought to be destroyed. Germophobia is big business in the United States: the market for antibacterial products—sanitizers, cleansing gels, cutting boards, and cotton swabs—grows larger every year. Even Disney offers its own brand of hand wipes, and so do the Yankees.
The impact is hard to dispute. An American born in 1930 could expect to die by the age of sixty; currently, the life expectancy of an infant is nearly seventy-nine years. There are many reasons for that remarkably rapid leap in longevity: the defeat of infectious diseases such as smallpox and polio; better standards of nutrition; readily available clean water; and, most important, perhaps, antibiotics. By the age of eighteen, the average American child has received from ten to twenty courses of antibiotics. Forty-three million courses were dispensed in 2010 alone, and throughout the developed world children receive, on average, at least one such treatment every other year. “Those drugs have saved countless lives, and it is very important that we not lose sight of that fact,’’ Blaser said. “Whenever they are used, though, there is collateral damage. And we are only now fully learning how severe that damage has been.”
At the beginning of the twentieth century, H. pylori occupied the stomach of nearly every person in the world. Although it remains prevalent in developing countries, where sanitation is often poor and antibiotic use less common, it is found in just five per cent of children born in the United States—a dramatic change echoed in many other Western countries. The relationship between H. pylori and disease has been well documented, but people rarely develop ulcers and stomach cancer early in life. During the past fifteen years, however, Blaser and a growing group of colleagues have shown that H. pylori performs beneficial functions that begin in infancy. In doing so, they have transformed the vanishing bacterium into a cautionary symbol of what can happen when we tinker with the ecological communities inside us. “This is just the best understood example,’’ Blaser told me. H. pylori is a complicated resident in our gut, and a reminder that the microbiome is dynamic, its constituents and effects changing over time. For some people, particularly as they age, H. pylori poses a serious threat. But in most cases it is commensal, the term scientists use to describe organisms that benefit from living on their hosts—us, in this case—without adverse effect. “There are specific circumstances under which Helicobacter can cause harm,’’ Blaser said, “but without it we are in real trouble.”
He pointed to asthma rates, which have risen rapidly in the developed world since the end of the Second World War, when antibiotics became widely available. The growth seems to have been matched by an equally sharp decline in the percentage of children infected with H. pylori. Coincidences like that are not rare in biology. (Causes and correlations are frequently confused. Vaccines have been mistakenly blamed for autism, for instance, because the condition often becomes apparent at about the time most children receive their largest cluster of vaccines. Nonetheless, no relationship between the two has ever been demonstrated.) Blaser conducted a larger and more targeted study. In 2007, after analyzing the Third National Health and Nutrition Examination Survey, in which more than seventy-five hundred adults participated, Blaser and his N.Y.U. colleague Yu Chen reported that people who didn’t have H. pylori in their guts were far more likely to have had asthma as children than those who did. Last year, Anne Müller, at the Institute of Molecular Cancer Research, at the University of Zurich, went further. She infected half of a cohort of mice with H. pylori, then exposed both groups to dust mites and to other, more severe allergens, in an effort to induce the cellular inflammation that is a hallmark of asthma. In every case, the mice without the bacterium became ill and those that carried it did not.
There is equally convincing evidence that destroying H. pylori could alter metabolism in ways that increase the risk of obesity. Several research groups, including Blaser’s, have found a strong relationship in humans between the bacterium and two stomach hormones, ghrelin and leptin, both of which play central roles in regulating our appetites. Like many hormones, they work as a team, telling us to eat when we are hungry and stop when we are full. The more ghrelin you have in your bloodstream, the more likely you are to overeat. Leptin functions in the opposite way, suppressing the appetite and increasing energy levels. For people whose stomachs are infected with H. pylori, ghrelin became far less detectable after a meal. For the others, levels of the hormone remained high, and the effects are evident. “A generation of kids are growing up without H. pylori regulating their levels of ghrelin,’’ Blaser told me. These results suggest that the message to stop eating never makes it to the brain. If those hormones aren’t controlled, it becomes far more difficult to control one’s weight.
A team from Blaser’s lab then fed antibiotics to mice in dosages that were comparable to those used to treat children with ear infections. The diet of the mice remained unchanged, but, compared with a control group, they gained considerable weight. That finding was not a complete surprise. Roughly three-quarters of the antibiotics consumed in the United States are fed to poultry, cows, and pigs, not to treat illness but as dietary supplements to promote faster growth. That saves the meat industry a lot of money; the sooner the animals reach a market weight, the sooner they can be slaughtered and sold. Until recently, the biochemical reasons for that weight gain, and its unsettling implications for humans, were murky. The new data suggest that even minimal exposure to antibiotics alters the gut bacteria of these animals, which may influence their ability to metabolize nutrients properly. As a result, researchers have concluded, both their body-fat percentage and their weight increase significantly.
In 2009, Blaser joined with the Stan ford microbiologist Stanley Falkow to write an essay titled “What Are the Consequences of the Disappearing Human Microbiota?,” which was published in the journal Nature Reviews Microbiology. It has been cited often, largely because the two provided a compelling answer to their own question. For the past hundred and fifty million years, nearly all mammals have acquired their microbiome by passing through their mother’s vagina, which is colonized by an enormous range of bacterial species. Babies delivered by Cesarean section lack many microbes that are routinely transferred from mother to child. Last year, nearly a third of the four million children born in the United States were delivered by Cesarean section. (In China, the figure was closer to fifty per cent.) The incidence of allergies and asthma is far higher among those children than it is for vaginal-birth babies. Moreover, this loss of microbial diversity appears to be cumulative. “The way we live now, we are losing these organisms, and each generation arrives with fewer than the one before,’’ Blaser said.
He took the theoretical case of a woman who was born at the turn of the twentieth century and possessed ten thousand species of bacteria. Beginning in the nineteen-thirties, with the advent of antibiotics, most people began to have one or two courses of antibiotics in their lives. After the war, hygiene improved as well. The result: fewer bacterial species in our microbiome. “Let’s say that the woman is down to nine thousand nine hundred and fifty,’’ he went on. “And then she has a daughter. That child is likely to take many more antibiotics than her mother did. She starts life with fewer species and she will lose more as she goes along.’’ Project this trend forward a few generations, and the implications are worrisome. “A lot of things are happening at once,’’ he said. “The rise in obesity, celiac disease, asthma, allergy syndromes, and Type 1 diabetes. Bad eating habits are not sufficient to explain the worldwide explosion in obesity.’’
Blaser walked me through the warren of his lab, where more than a dozen students, scholars, postdocs, and colleagues from Japan, Mexico, and Sweden, among other countries, were working on this problem. We stared at computer screens filled with detailed pictures of mice so enormous they looked like floats in the Macy’s Thanksgiving Day Parade; they had all been fed steady, low doses of antibiotics. “We are not talking about illnesses that are increasing by ten per cent,’’ Blaser said. “They are doubling and tripling and quadrupling. With each generation, there is a heavier impact on the early-life microbiome. And it means we are less and less able to metabolize the food we eat.”
Andrew Goldberg, who is the director of rhinology and sinus surgery at the U.C.S.F. Medical Center, likes to tell a story about earwax. One day in 1986, when he had just begun a residency at the University of Pittsburgh School of Medicine, a man walked into the clinic. The patient had been there many times before, always for the same reason—a chronic infection in his left ear. Stubborn ailments like that are common, though they usually occur in both ears.
“It was one of those refractory cases,” Goldberg told me recently. “The doctors had tried everything: several types of antibiotics, antifungal drops, the works. That was standard practice, and we were proud of ourselves for doing it.” Goldberg and I sat one chilly August afternoon in a coffee shop across from his office, in the Clinical Sciences Building. He spoke almost wistfully, as if recalling an antiquated practice, like bloodletting. Despite repeated treatments, the man’s ear had not improved. But on this day he walked into the clinic with a smile, and Goldberg soon saw why: the ear looked great. “I have not felt this well in years,’’ the patient said. “Do you want to know what I did?” The doctor assumed that one of the drugs had finally found its mark. “I took some wax out of my good ear and put it into my bad ear, and in a few days I was fine,” the patient said.
“I thought he was nuts,’’ Goldberg told me. He never gave the encounter another thought—until a couple of years ago, when he began to investigate the causes of those common ear infections. Goldberg explained that earwax contains many bacterial species and that antibiotics might have destroyed one or more in his bad ear. “It was actually something like a eureka moment,’’ he said, chuckling. “I realized that this patient was the perfect experiment: a good ear and a bad ear separated by a head. That guy wasn’t crazy; he was right. Clearly, he had something protecting one ear that he then transferred to the other ear. Drugs didn’t cure him. He cured himself.”
Goldberg worries about the modern reliance on antibiotics. “We have always had this scorched-earth policy,” he continued. One of his research specialties is chronic sinusitis, which is the fifth most common reason people take antibiotics. “The annual economic burden is more than two billion dollars,” he said. Goldberg and his associates at U.C.S.F. have found that the sinus passages of a person with sinusitis are typically inhabited by some nine hundred strains of bacteria. Remarkably, a healthy person has even more—twelve hundred species. “Our contention is that other elements of the bacterial community are keeping the infection in check,” Goldberg said. “Those microbes are the equivalent of the good earwax. And for eighty years we have done everything in our power to get rid of all of them.”
It’s going to take time, and much more research, before bacteria are used as if they were drugs. But for clinicians like Katherine Lemon the future can’t arrive soon enough. Lemon is a microbiologist on the staff of the Forsyth Institute, in Cambridge; an infectious-disease specialist at Boston Children’s Hospital; and an assistant professor of pediatrics at Harvard Medical School. Along with Michael Fischbach, an assistant professor in the Department of Bioengineering and Therapeutic Sciences at U.C.S.F., and others, Lemon is trying to understand why bacteria infect some people but not others. One of her projects revolves around a curious fact: thirty per cent of Americans are vulnerable to a wide range of infections, it appears, because Staphylococcus aureus bacteria colonize in their nostrils. But seventy per cent don’t harbor that microbe; Lemon is trying to discover how the good bacteria manage to keep the staph out.
“One of these days—not tomorrow, but I hope not in the distant future—we will sample the microbiome of every child the first time his parents bring him to the doctor,” Lemon said. Lemon, who is forty-seven, has a square face and graying hair that constantly seems to fall into her eyes. We were talking in her office at Forsyth, which was founded more than a century ago as a dental clinic for underprivileged children. It has since expanded its focus. “We will do what we do now: take blood, administer vaccines, run the usual tests,” she said. “But we will have this invaluable extra tool of being able to understand how children’s microbial communities develop.
“And I can envision a conversation with the parents,’’ she went on, “where the pediatrician would say, ‘Your child’s blood work is fine. She is hitting all her milestones and she looks great. But after seeing her gut microbiome, given the history of inflammatory-bowel disease in your family, I would like to prescribe a probiotic that can help populate her intestines with the proper combination of microbes.’ ” In order to do that, of course, Lemon and other scientists will have to agree upon what a healthy microbiome looks like. Since the bacteria in our bodies change throughout our lives, the task will not be simple.
Last year, however, researchers led by Peer Bork, of the European Molecular Biology Laboratory, in Heidelberg, discovered that people can be classified by the type of bacterial species that dominate their guts. The group found that humans fall into one of three categories—called enterotypes—none of which correlate to age, race, or gender. The finding, analogous to the discovery, a century ago, that there are four blood types, could eventually help lead to treatments. “Some things are pretty obvious already,’’ Bork told the Times when the research was published. “Doctors might be able to tailor diets or drug prescriptions to suit people’s enterotypes.” He added that, instead of prescribing antibiotics, a doctor might, on the basis of these categories, restore bacteria that had been destroyed. As many as forty per cent of children treated with a broad-spectrum antibiotic will develop a condition called pediatric antibiotic-associated diarrhea. Several clinical trials have now indicated that the use of probiotics during antibiotic treatment might prevent this disease.
“It’s early work but very promising,’’ Lemon told me. “And there is even more hopeful research in other areas.” About ten per cent of people carry a bacterium called Clostridium difficile. The bacterium is normally held in check by other residents of the gut. But when those companion bacteria are destroyed by antibioticsC. difficile can erupt, causing severe diarrhea and deadly inflammation in the colon. Nearly every C. difficile infection occurs as a result of antibiotic treatment, and the incidence has risen sharply in the U.S. in the past twenty years. The infection causes tens of thousands of deaths in the world, and hundreds of thousands of illnesses among hospital patients. Most patients recover; many need several additional courses of antibiotics. For some, the destruction of their microbiome has been so severe that no treatment seems to work. “Those patients suffer terribly,’’ Lemon told me. “They are in agony and, really, there has been nothing to do but try to treat their condition every time it returns.’’
Recently, out of desperation as much as anything else, researchers have resorted to what seems like an extreme treatment: fecal transplants. Doctors obtain fecal bacteria from healthy donors—normally family members—and place them in the patient’s intestines, usually during a colonoscopy. There have been only a few brief trials, but the results have been astounding. In one study, all thirty-four recipients were cured; these are people for whom all other approaches had failed. Other trials have reported success rates of more than eighty per cent. “There are obviously other diseases that could be susceptible to this kind of microbial therapy,’’ Lemon said; she mentioned inflammatory-bowel disease, allergies, and recurring ear infections. The hope is that someday researchers will treat bacteria with highly specific antibiotics and then rebuild our damaged ecosystem with probiotics—strains of bacteria that could act as surrogate farmers in our internal ecosystems. One study, in mice, showed that the toxic side effects of a colon-cancer drug were eased by blocking a particular bacterial enzyme. “It’s promising,’’ Lemon told me. “But we need to move very carefully to confirm the results when they look so good.”
Late one night, while flipping through television channels, I came upon an advertisement for a probiotic called Culturelle. After a tag line, “Bacteria Is Beautiful,’’ the ad featured satisfied customers who testified to the “awesome” relief they obtained from diarrhea, constipation, and other digestive ailments. This, the manufacturer suggested, is because Culturelle offers “Lactobacillus GG, the good bacteria,” which has been “clinically shown to improve your digestive health.”
The promise of microbiome research rests largely on the future of probiotics, but so far such treatments have been more useful as experimental tools than as medicine. That fact has not deterred the hucksters. Sales of probiotic foods and supplements have quadrupled since 1998, and it is estimated that they will grow even faster during the next few years. It’s nearly impossible to walk into a grocery store without encountering some product described as a “probiotic.” (My local store, for instance, offers such samplings as Renew Life’s Ultimate Flora Plus Fiber, for digestive relief, which the box says contains ten billion live cultures; Ultimate Flora Adult Formula, with fifteen billion live cultures per capsule; and Ultimate Flora Critical Care, with fifty billion cultures in a single pill.) “I am hopeful about the future of probiotics,’’ Blaser told me. “But they have to be based on science. Current products are ninety-nine per cent marketing.”
The Culturelle ad claims that its active ingredient, Lactobacillus GG, has been shown to “survive those good-bacteria-gobbling stomach acids and successfully stick to the intestinal walls where it’s needed most.” Studies have indicated that Lactobacillus GG is indeed a “good” bacterium—most of the time. But the relationship between humans and our microbial tenants is never simple. The American Academy of Microbiology, for example, has reported that although Lactobacillus GG appears to reduce the risk of eczema in babies, it can worsen the condition of people with Crohn’s disease, and in rare cases it could cause endocarditis, a potentially deadly inflammation of the inner layers of the heart.
Eventually, it may become possible to restore the health of a depleted microbiome simply by swallowing a capsule crammed with billions of bacterial cells, or by eating yogurt. At the moment, however, not a single probiotic for sale in the United States has been approved as a drug; instead, probiotics are sold as dietary supplements or as foods like yogurt. This permits supplement manufacturers to make almost any claim about the benefits of the products as long as the packaging includes, usually in the tiniest possible type, this disclaimer: “These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.”
That kind of latitude gives customers little guidance. Joseph Mercola maintains one of the most popular alternative-health Web sites in America, and he is particularly bullish on probiotics. Without offering any evidence, his Web site tells potential customers that if you buy his Complete Probiotics, and take two capsules “15-30 minutes prior to eating breakfast,” you will give “70+ billion colony-forming units time to prep your digestive system for what you’re about to eat.’’ Complete Probiotics contains ten strains of bacteria, and Mercola’s logic, shared by many other manufacturers, seems to be that if each of the strains is beneficial on its own it will be that much more powerful when combined with others.
“That argument is fallacious, and potentially very troublesome,” Michael Fischbach, of U.C.S.F., told me. He noted that although some antibiotics, taken together, enhance each other’s effectiveness, the opposite is also true: some common drugs are deadly when combined. “Therapeutics based on bacterial cells will never take off until physicians feel confident that they can prescribe them as medicine, without problems,’’ Fischbach said. “Right now, the standard for evidence is disgustingly low. If we expect the knowledge we gain from the microbiome to transform human health, that will have to change. If not, probiotics will be nothing more than snake oil.”
This week, Martin Blaser will address a plenary session of the Infectious Diseases Society of America, an organization that he once led. The title of his talk, “The Menace of Antibiotics,” would have generated guffaws and outrage twenty years ago. Even today, it is easy to misconstrue his message. “We are an endlessly variable stew of essential microbes,’’ he told me. “And they are working in ways we have not yet understood. Antibiotics are so miraculous that we have been lulled into a belief that there is no downside. But there is: they kill good bacteria along with the bad bacteria.” The implication is that good bacteria actually act as antibiotics—and are often more effective that those we buy at a drugstore. But the microbiome is never static or simple; often it’s a battleground between species. The difficult job of medicine is to control that battleground.
Whether a microbe like H. pylori is dangerous or beneficial will always depend on the ecological context in which it is found. In 1998, Blaser was asked by the British Medical Journal to contribute to a special series devoted to the future of medicine. He wrote that one day doctors would begin to give Helicobacter pylori back to children—so that they would have them, just as our ancestors did. “I am more convinced of that today than I have ever been,’’ he said. “We will need to make sure that pregnant women have the appropriate microbial communities to pass on to their children. If they don’t, we will have to give them to the kids after they are born. Then, for certain bacteria, like Helicobacter, at the age of thirty or forty, they could go to a clinic and have them eradicated. That way, people can get the benefit of these organisms in early life without having to pay the cost as they age.
“This has got to be an important part of the future of medicine,” he said. “Nothing else makes sense.” ♦
***
"10,000 Germs and a Few Pounds of Bacteria is Healthy"
Fox News